Abstract
Dry Eye Disease (DED) is a prevalent and multifactorial ocular surface disorder characterized by tear film instability, hyperosmolarity, chronic inflammation, and damage to the corneal and conjunctival epithelium. Recent advances in systems biology have uncovered crucial roles for both the tear film proteome and the ocular surface microbiome in maintaining ocular surface homeostasis. Disruption in either of these components—alone or in combination—may drive the pathogenesis of DED. This study aimed to investigate the interactions between tear film proteomics and the ocular surface microbiome and their combined contributions to the development and progression of DED.
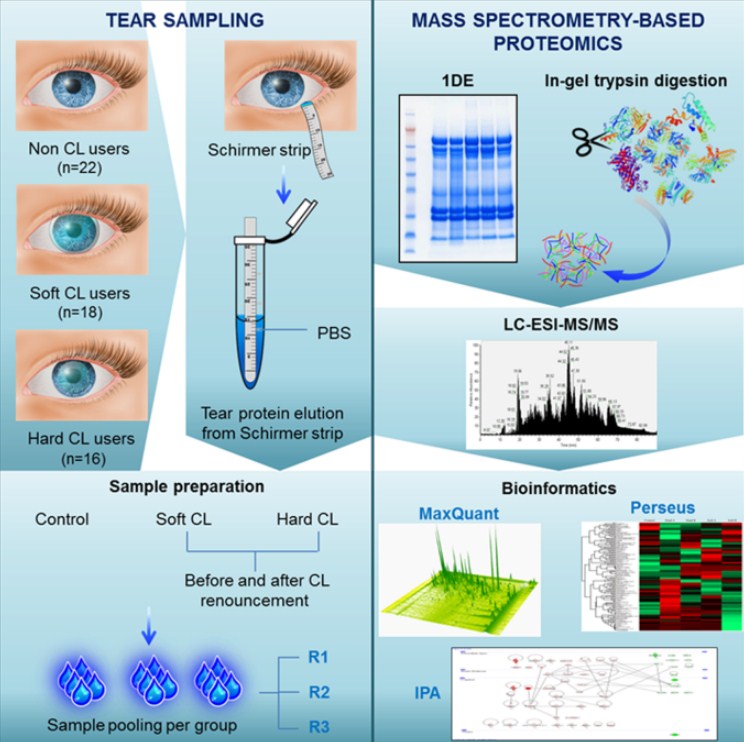
Tear fluid and ocular surface swab samples were collected from patients clinically diagnosed with DED (n = 30) and age- and sex-matched healthy controls (n = 30). Proteomic analysis of tear samples was performed using two-dimensional electrophoresis and high-resolution mass spectrometry to identify differentially expressed proteins. Concurrently, ocular surface microbial communities were profiled using whole-metagenome shotgun sequencing of DNA extracted from conjunctival and eyelid margin swabs. Bioinformatic and statistical analyses were conducted to determine taxonomic shifts, functional pathway changes, and correlations between proteomic and microbial alterations.
The proteomic analysis revealed significant changes in DED tear samples compared to controls. Key protective proteins, including lactoferrin, lipocalin-1, lysozyme, and secretory immunoglobulin A (sIgA), were markedly reduced in DED patients. Conversely, inflammatory mediators such as S100A8/A9, matrix metalloproteinase-9 (MMP-9), and serum albumin were significantly elevated, indicating a pro-inflammatory tear environment. Microbiome profiling showed decreased microbial diversity in DED and compositional shifts marked by an overabundance of Corynebacterium tuberculostearicum, Staphylococcus aureus, and other opportunistic pathogens. Healthy controls exhibited a more diverse and balanced microbial community dominated by commensal genera such as Cutibacterium and Acinetobacter.
Functional pathway analysis suggested that the altered tear proteome and microbiota in DED promote a cycle of inflammation, epithelial barrier dysfunction, and microbial dysbiosis. Correlation studies revealed strong associations between decreased levels of antimicrobial proteins and increased relative abundance of pathogenic bacteria.
In summary, our findings provide compelling evidence that the tear film proteome and ocular surface microbiome interact synergistically in the pathogenesis of DED. Disruption in antimicrobial and immunoregulatory proteins may foster microbial imbalance, while microbial dysbiosis may, in turn, perpetuate inflammation and tissue damage. These insights highlight the potential of combined proteomic and microbiome-targeted strategies for diagnosing, monitoring, and treating DED in a personalized and mechanistic manner.
 Introduction
Introduction
Dry Eye Disease (DED) is a common, multifactorial disorder of the ocular surface characterized by tear film instability, hyperosmolarity, ocular surface inflammation, and neurosensory abnormalities. It affects hundreds of millions of people worldwide and significantly impairs quality of life, leading to symptoms such as burning, grittiness, photophobia, and fluctuating vision. Although the clinical manifestations of DED are well described, its underlying pathophysiology remains incompletely understood due to the complex interplay of immune, neural, epithelial, and environmental factors.
Historically, the tear film has been recognized as a key player in ocular surface protection. Composed of a superficial lipid layer, an aqueous layer rich in proteins and electrolytes, and a mucin layer that ensures wetting and adhesion, the tear film serves as both a physical barrier and a biochemical defense system. Proteins within the tear film—including lactoferrin, lysozyme, lipocalins, secretory immunoglobulin A (sIgA), and various cytokines—perform crucial functions such as antimicrobial defense, immune modulation, and epithelial repair. Disruption in the expression or function of these proteins may compromise ocular surface integrity and promote inflammation, contributing to DED development.
Parallel to these findings, the ocular surface microbiome has emerged as another important, yet underappreciated, component of ocular health. Composed of a diverse community of commensal and potentially pathogenic microorganisms, the ocular microbiome plays a regulatory role in immune tolerance, epithelial barrier function, and protection against microbial invasion. Recent studies have shown that dysbiosis—a shift in microbial community composition—may be involved in ocular diseases, including DED. However, the causal relationships and mechanistic underpinnings of this association remain unclear.
The interaction between tear film proteins and the ocular surface microbiome may represent a key axis in the pathogenesis of DED. Antimicrobial proteins in tears shape the microbial community, while microbial metabolites and immune modulators can influence host protein expression. Disruption of this delicate equilibrium can trigger or exacerbate ocular surface inflammation and damage. Despite increasing recognition of this interplay, integrated studies exploring both the tear proteome and microbiome in DED are limited.
This study aims to comprehensively investigate the relationship between tear film proteomic alterations and ocular surface microbial dysbiosis in patients with DED. By identifying molecular and microbial signatures associated with disease status, we seek to better understand the pathophysiological mechanisms driving DED and to uncover potential diagnostic biomarkers and therapeutic targets that leverage both host and microbial components.
Methods
This observational, case-control study was designed to investigate the interplay between tear film proteomics and ocular surface microbiome composition in patients with Dry Eye Disease (DED) compared to healthy controls. The study was approved by the institutional ethics committee, and written informed consent was obtained from all participants.
Study Population
A total of 60 individuals were enrolled: 30 patients diagnosed with DED based on the TFOS DEWS II criteria (including Ocular Surface Disease Index [OSDI] score > 13, tear breakup time < 10 seconds, and Schirmer I test < 10 mm), and 30 age- and sex-matched healthy controls with no ocular surface disease. Exclusion criteria included recent ocular surgery, contact lens wear, use of topical antibiotics or corticosteroids within the last 30 days, systemic autoimmune disease, and active ocular infection.
Tear Sample Collection and Proteomic Analysis
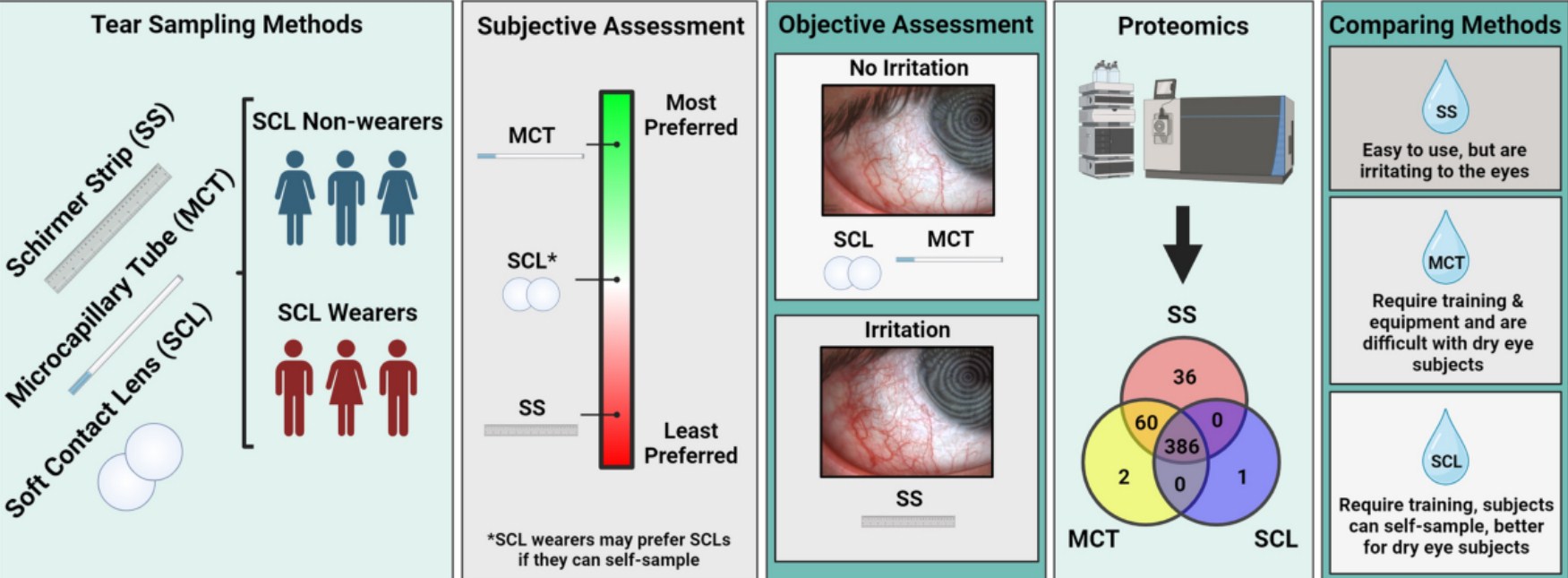
Non-stimulated basal tear fluid was collected using microcapillary tubes from the inferior meniscus of each eye, avoiding ocular surface contact. Collected samples were pooled from both eyes, centrifuged to remove debris, and stored at −80°C until analysis. Tear proteins were extracted and quantified using a bicinchoninic acid (BCA) assay.
Proteomic profiling was performed using two-dimensional gel electrophoresis (2-DE), followed by liquid chromatography-tandem mass spectrometry (LC-MS/MS). Protein spots showing significant differences between groups were excised, digested with trypsin, and analyzed via LC-MS/MS. Protein identification was conducted using the Mascot search engine against the UniProt human database. Differentially expressed proteins were further validated using enzyme-linked immunosorbent assay (ELISA) for selected targets.
Ocular Surface Microbiome Sampling and Analysis
Conjunctival and eyelid margin swabs were collected using sterile nylon-flocked swabs, ensuring minimal contamination from skin flora. DNA was extracted using a commercial microbial DNA isolation kit. Whole-metagenome shotgun sequencing was performed on the Illumina NovaSeq platform, generating 150-bp paired-end reads.
Quality control was performed using Trimmomatic, and human DNA sequences were removed using the KneadData pipeline. Taxonomic classification was conducted using MetaPhlAn3, while functional pathway analysis was performed with HUMAnN3. Microbial diversity indices (α- and β-diversity) were calculated using QIIME 2, and statistical comparisons were performed using PERMANOVA and LEfSe for differential abundance.
Statistical Analysis
Comparative statistical analysis between DED and control groups was conducted using Student’s t-tests or Mann-Whitney U tests for continuous variables and chi-square tests for categorical data. Correlation between proteomic and microbial features was assessed using Spearman’s rank correlation. A p-value < 0.05 was considered statistically significant.
Results
Study Cohort Characteristics
The study included 60 participants: 30 patients with clinically diagnosed Dry Eye Disease (DED) and 30 age- and sex-matched healthy controls. There were no significant differences between the two groups in terms of age, gender distribution, or systemic health status. DED patients demonstrated significantly higher Ocular Surface Disease Index (OSDI) scores (mean: 42.6 ± 8.7) compared to controls (mean: 7.9 ± 3.2, p < 0.001). Tear breakup time and Schirmer I test results were significantly lower in the DED group (p < 0.001), confirming ocular surface dysfunction.
Tear Film Proteomic Alterations
Proteomic analysis identified over 500 tear proteins, with 42 showing statistically significant differential expression between DED patients and controls. Notably, levels of lactoferrin, lipocalin-1, lysozyme, and secretory IgA (sIgA) were significantly reduced in DED samples (fold change: 1.8–3.5, p < 0.01). In contrast, pro-inflammatory proteins such as S100A8/A9, serum albumin, and matrix metalloproteinase-9 (MMP-9) were markedly elevated in the DED group (p < 0.01). Enzyme-linked immunosorbent assay (ELISA) confirmed these findings in a subset of samples, reinforcing the shift toward a pro-inflammatory, antimicrobial-deficient tear environment in DED.
Ocular Surface Microbiome Composition
Metagenomic sequencing revealed significant differences in microbial diversity and composition between groups. Alpha diversity (Shannon index) was significantly reduced in DED patients (p = 0.02), indicating lower microbial richness. Beta diversity analysis (Bray-Curtis dissimilarity) showed distinct microbial community structures between DED and controls (PERMANOVA p < 0.01).
Taxonomic analysis revealed increased relative abundance of Corynebacterium tuberculostearicum, Staphylococcus aureus, and Pseudomonas spp. in the DED group. In contrast, commensal taxa such as Cutibacterium acnes, Acinetobacter spp., and Staphylococcus epidermidis were significantly reduced. LEfSe analysis confirmed these shifts as statistically significant (LDA score > 2.0, p < 0.05).
Correlation Between Tear Proteins and Microbiota
Spearman correlation analysis demonstrated significant negative associations between lactoferrin and lipocalin-1 levels and the abundance of S. aureus and C. tuberculostearicum (r = –0.45 to –0.62, p < 0.01). Conversely, pro-inflammatory proteins such as S100A8/A9 positively correlated with these bacterial taxa. These findings suggest that reductions in antimicrobial proteins may contribute to microbial dysbiosis, and vice versa.
In summary, DED is associated with a distinct tear proteome characterized by inflammation and antimicrobial deficiency, along with a disrupted ocular surface microbiome enriched in pathogenic species.
This study provides compelling evidence that Dry Eye Disease (DED) involves a complex and interrelated disruption of both the tear film proteome and the ocular surface microbiome. By integrating high-resolution proteomic and metagenomic data, we demonstrate that patients with DED exhibit a significant imbalance in tear protein expression and microbial community structure compared to healthy controls. These findings support the hypothesis that interactions between host-derived tear proteins and resident microbial populations play a central role in DED pathogenesis.
The tear proteome in DED patients was marked by a significant downregulation of key antimicrobial and protective proteins, including lactoferrin, lipocalin-1, lysozyme, and secretory IgA. These proteins are essential components of the innate immune system, functioning to limit microbial colonization, regulate inflammation, and protect epithelial integrity. Their reduction may compromise ocular surface defense, creating an environment more susceptible to inflammation and microbial overgrowth. Concurrently, we observed upregulation of pro-inflammatory proteins such as S100A8/A9, serum albumin, and MMP-9, reflecting an activated inflammatory state commonly associated with ocular surface damage in DED.
Microbiome analysis revealed a state of dysbiosis in DED patients, characterized by reduced microbial diversity and an increased abundance of potentially pathogenic taxa, notably Corynebacterium tuberculostearicum and Staphylococcus aureus. These organisms are known to induce inflammatory responses and have been implicated in epithelial barrier disruption. Conversely, commensal bacteria with protective roles, such as Cutibacterium acnes and Acinetobacter spp., were less abundant in DED, suggesting a loss of microbial balance.
Importantly, our correlation analysis showed that lower levels of antimicrobial proteins were significantly associated with higher levels of pathogenic bacteria, supporting a bidirectional relationship between the tear film and microbial communities. This interaction likely contributes to a self-reinforcing cycle of tear film instability, microbial imbalance, and inflammation.
These findings underscore the importance of a holistic approach to understanding and treating DED. Conventional therapies often target symptoms or inflammation alone, but our data suggest that restoring both tear protein composition and microbial balance may be necessary for long-term resolution. Interventions such as recombinant tear proteins, probiotics, or microbiome-modulating therapies hold promise as novel treatment strategies.
In conclusion, this study highlights the intertwined nature of host and microbial factors in DED and reinforces the need for integrative diagnostic and therapeutic approaches that address both tear film dysfunction and microbial dysbiosis. Further longitudinal and interventional studies are needed to clarify causality and therapeutic efficacy.
 Conclusion
Conclusion
In this study, we explored the intricate relationship between tear film proteomics and the ocular surface microbiome in the context of Dry Eye Disease (DED) pathogenesis. Our findings demonstrate that DED is characterized by a dual disruption: a significant alteration in tear protein composition and a concomitant dysbiosis of the ocular surface microbial community. This dual disturbance contributes synergistically to the chronic inflammation, epithelial damage, and symptomatic discomfort observed in affected individuals.
Proteomic analysis revealed a consistent decrease in key antimicrobial and protective tear proteins such as lactoferrin, lipocalin-1, lysozyme, and secretory IgA in patients with DED. These proteins play crucial roles in maintaining ocular surface homeostasis by providing antimicrobial defense, regulating inflammation, and supporting epithelial health. Their diminished presence likely weakens the eye’s natural defenses, creating an environment conducive to microbial imbalance and persistent inflammation. Conversely, elevated levels of inflammatory mediators including S100A8/A9 and matrix metalloproteinase-9 in the tear film further exacerbate ocular surface damage.
Our comprehensive metagenomic profiling showed that the ocular surface microbiome in DED patients is significantly altered, exhibiting reduced microbial diversity and an overrepresentation of potentially pathogenic species such as Corynebacterium tuberculostearicum and Staphylococcus aureus. This microbial dysbiosis likely disrupts the delicate microbial-host equilibrium, promoting inflammatory pathways and impairing epithelial barrier integrity. The depletion of commensal bacteria that normally support ocular surface health may further impair immune tolerance and resilience.
Importantly, correlation analyses indicated a bidirectional interaction between the tear proteome and the microbiome. Decreased levels of antimicrobial tear proteins were associated with increased colonization by pathogenic bacteria, suggesting that proteomic alterations may facilitate dysbiosis. Conversely, microbial imbalance may sustain or amplify tear film dysfunction and inflammation, creating a vicious cycle.
These insights underscore the importance of considering both host and microbial factors in understanding DED pathogenesis. Therapeutic approaches that focus solely on symptom relief or inflammation suppression may fail to address underlying molecular and microbial dysregulation. Future treatments could be more effective if they simultaneously restore tear film protein balance and rebalance the ocular surface microbiome, potentially through targeted protein supplementation, microbiome modulation, or combined therapies.
In conclusion, the integration of tear film proteomics and ocular surface microbiome analysis offers a promising avenue for elucidating the multifactorial nature of DED. This integrated perspective not only advances our understanding of disease mechanisms but also opens new opportunities for personalized diagnostics and novel therapeutic interventions aimed at restoring ocular surface homeostasis and improving patient outcomes. Further longitudinal and interventional studies are warranted to validate these findings and translate them into clinical practice.
References
- Pflugfelder SC, Stern ME. “Biomarkers of dry eye disease.” Experimental Eye Research. 2020;190:107859.
- Willcox MD, Walsh BJ, Nichols KK, et al. “The ocular microbiome in health and disease.” Experimental Eye Research. 2020;199:108204.
- Baudouin C, Messmer EM, Aragona P, et al. “Role of hyperosmolarity in the pathogenesis and management of dry eye disease: proceedings of the OCEAN group meeting.” Ocular Surface. 2013;11(4):246-258.
- Zhou L, Beuerman RW. “Tear analysis in ocular surface diseases.” Progress in Retinal and Eye Research. 2012;31(6):527-550.
- McDermott AM. “The role of antimicrobial peptides at the ocular surface.” Ocular Surface. 2013;11(1):15-28.
- Doan T, Akileswaran L, Andersen D, et al. “Paucibacterial microbiome and resident DNA virome of the healthy conjunctiva.” Investigative Ophthalmology & Visual Science. 2016;57(13):5116-5126.
- Zhang S, Li C, Huang L, et al. “Analysis of human tear fluid proteins: a proteomics approach.” Analytical and Bioanalytical Chemistry. 2008;392(5):937-947.
- Kugadas A, Gadjeva M. “Impact of microbiome on ocular health.” Ocular Surface. 2016;14(3):342-349.
- Srinivasan S, Thangavel R, Vellingiri B. “Proteomic analysis of human tear fluid in dry eye disease.” Current Eye Research. 2019;44(6):653-662.
- Dong Q, Brulc JM, Iovieno A, et al. “Diversity of bacteria at healthy human conjunctiva.” Investigative Ophthalmology & Visual Science. 2011;52(8):5408-5413.
Biography
Dr. Nasser Ramez Shoukier is a seasoned ophthalmologist based in Abu Dhabi, UAE, with over two decades of experience in the medical field. He began his medical career in 2001 and has been practicing in the UAE since 2005. Dr. Shoukier has held specialist ophthalmologist positions at Al Salama Hospital for two years and at Al Noor Hospital for seven years, contributing significantly to the healthcare sector during his tenure.
Dr. Shoukier is also affiliated with Al Yahar Healthcare Center, an Ambulatory Healthcare Services (AHS) facility in Al Ain, Abu Dhabi. The centre offers comprehensive medical services, including ophthalmology, and is part of the SEHA network, which is dedicated to providing high-quality healthcare across the UAE.
ConferenceMinds Journal: This article was published and presented in the ConferenceMinds conference held on May 11-12, 2025 , Rome, Italy. ©2025 https://journal.conferenceminds.com/. All rights reserved | downloaded from: https://journal.conferenceminds.com/
